- 617-525-8128
- AVMsurgeon@bwh.harvard.edu
- 75 Francis St, Boston, MA 02115, USA
Understanding AVM treatment can be challenging. That’s why we’ve curated a collection of real surgical procedures, patient journeys, and expert case studies. These videos provide in-depth insights into how AVM is diagnosed, treated, and managed by leading specialists.
Browse our gallery to explore groundbreaking procedures and success stories.
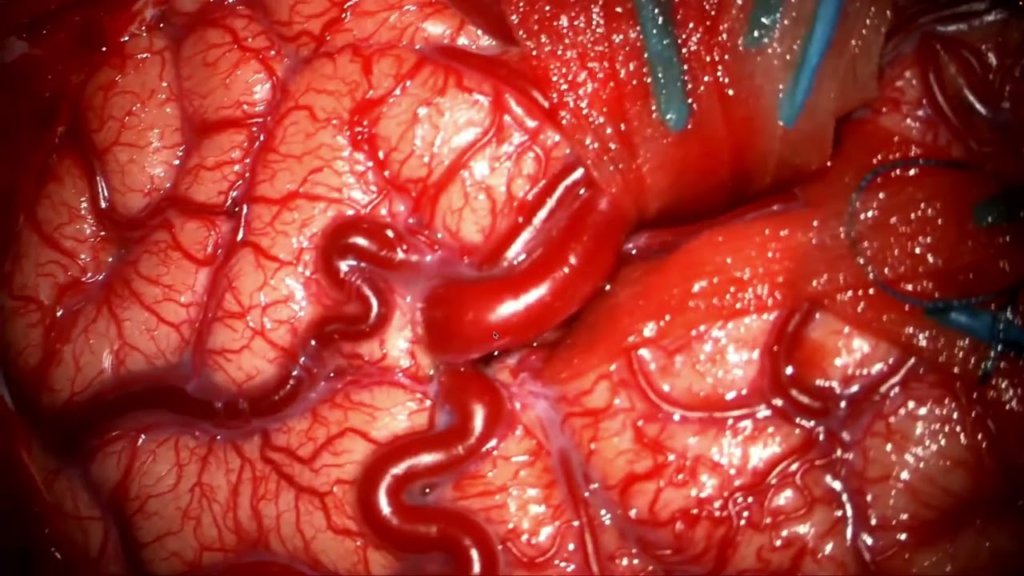
This surgical video demonstrates the step-by-step microsurgical resection of an arteriovenous malformation (AVM) located in the occipital lobe. The AVM was fed by branches of the MCA, ACA, PCA, and dural arteries, and was approached via a bilateral transfalcine route with the patient in a supine position. The video highlights meticulous arachnoid dissection, temporary clipping of feeders to reduce AVM pressure, and deep white matter dissection to isolate the nidus. Once the arterial inflow was controlled, the nidus was safely mobilized and resected. Final hemostasis was achieved, and the patient had no permanent neurological deficits. Postoperative angiography and follow-up MRI confirmed complete AVM removal.
This case study presents a detailed surgical approach to the resection of a high-grade brain arteriovenous malformation (AVM) using advanced brain mapping techniques. The procedure involves a semisitting supine biparietal craniotomy, intraoperative angiography, and neurophysiological monitoring to ensure precise navigation around critical eloquent areas, including the corticospinal tracts and visual pathways.
The surgical strategy focuses on stepwise vascular control, subcortical mapping, and meticulous dissection to optimize patient outcomes while minimizing neurological deficits.
Dr. Nirav J. Patel, a cerebrovascular surgeon at Brigham and Women’s Hospital, presents a case involving a 23-year-old woman with a ruptured arteriovenous malformation (AVM) in the motor cortex. The AVM is an abnormal connection of arteries and veins without capillaries, causing a risk of bleeding.
The surgical procedure involves a craniotomy followed by meticulous dissection under a microscope to isolate and remove the AVM while preserving surrounding brain structures. The key steps include:
Successful AVM Resection in Paraguay: Advancing Neurosurgical Care
Dr. Patel shares the successful resection of a ruptured vermian arteriovenous malformation (AVM) in an eight-year-old boy in Paraguay. The procedure, performed with meticulous precision, involved careful control of key feeding arteries and a stepwise dissection to ensure a safe and complete removal. Postoperatively, the child recovered without deficits and was eager to resume daily activities.
This milestone marks the beginning of a sustainable AVM treatment program in Paraguay, utilizing local resources and refining surgical techniques to improve patient outcomes.
Dr. Nirav Patel details the successful resection of a complex, previously ruptured AVM in a 37-year-old patient in Paraguay. The meticulous approach involved early identification and control of feeding arteries, careful dissection of the nidus, and a strategic resection to minimize risks. Postoperative imaging confirmed complete removal, with no residual AVM.
This case highlights the effectiveness of advanced neurosurgical techniques in resource-limited settings, reinforcing the commitment to improving AVM treatment in Paraguay.
The Brigham Neurosurgery team traveled to Paraguay to perform life-changing brain AVM surgeries and establish a sustainable neurosurgical program.
Led by Dr. Nirav J. Patel, this mission combined expertise, innovation, and collaboration to overcome resource limitations and provide high-quality care.
Watch as they navigate complex procedures, train local teams, and make a lasting impact.